 In theory, it should be useful to understand the factors predictive of poor adherence to PAP treatment and thus allow targeting of patients at high risk for treatment failure. Predictive factors have not been completely consistent between studies, but in general factors found to increase PAP adherence are increased severity of sleep apnea, greater daytime sleepiness, perceived symptomatic benefit, and a higher AHI. Factors that negatively influence adherence are lack of daytime sleepiness, lack of perceived benefit, side effects from PAP, previous uvulopalatopharngoplasty, nasal obstruction, and claustrophobia. Of interest, studies have not found pressure level to be predictive of adherence.
In theory, it should be useful to understand the factors predictive of poor adherence to PAP treatment and thus allow targeting of patients at high risk for treatment failure. Predictive factors have not been completely consistent between studies, but in general factors found to increase PAP adherence are increased severity of sleep apnea, greater daytime sleepiness, perceived symptomatic benefit, and a higher AHI. Factors that negatively influence adherence are lack of daytime sleepiness, lack of perceived benefit, side effects from PAP, previous uvulopalatopharngoplasty, nasal obstruction, and claustrophobia. Of interest, studies have not found pressure level to be predictive of adherence.
A number of social cognitive models have been applied to the treatment of chronic disease including PAP treatment. In one model of chronic disease, the patient’s perception of the relative weight of costs (side effects, inconvenience) vs benefits (symptom improvement) is viewed as determining adherence. Using social cognitive theory, several components have been hypothesized to be relevant to CPAP adherence: (1) perception of risk from untreated sleep apnea, and (2) expectations regarding treatment outcome (outcome expectancies) and confidence or volition to engage in treatment behavior (treatment self-efficacy). This model provides a means of assessing factors predictive of poor adherence and provides a structure for the design of more effective interventions.
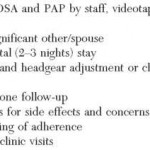
A number of prospective studies have tried to document improvements in adherence by various interventions. A problem with these studies’ is that many used a “package” of interventions so that the importance of each individual component cannot be determined. A list of techniques that alone or as part of a systematic approach have been shown to improve adherence are listed in Table 4. Simple interventions using the telephone can increase ad-herence, and group education provides a cost-effective intervention. Early and frequent initial follow-up after PAP initiation to troubleshoot problems with PAP usage, and at least yearly follow-up thereafter is recommended. It is possible that multidisciplinary PAP adherence clinics involving respiratory therapists, sleep physicians, otolaryngologists, and sleep psychologists may improve the adherence significantly.
Better evidence of the long-term benefits of PAP treatment is needed to support our recommendation that PAP should be used even in the absence of significant symptoms when severe sleep apnea is present. Identification of those patients who are most likely to accrue health benefits from PAP and more information on the amount of use required for benefit would be extremely useful. An example of the type of study needed is the Apnea Positive Pressure Long-term Efficacy Study, a current multicenter study, with the goal of determining the size, time course, and durability of the effects of long-term CPAP treatment on neurocognitive function, mood, sleepiness, and quality of life.
It is also imperative that technologies continue to improve comfort and convenience (device size and noise) of PAP treatment. Additional improvements in PAP interfaces are still needed. Is it realistic to expect that three to six sizes of a mask will work with the large spectrum of facial contours? Change in policies controlling reimbursement for PAP interfaces to make allowance for several mask changes at the initiation of treatment would be very useful. The optimal approach to the treatment of sleep apnea may benefit from information gained in treating other chronic diseases (for example: Chronic Obstructive Airway Disease). The lack of coordination between sleep centers, physicians, and durable medical equipment providers must be eliminated. Studies documenting the value of integrated PAP delivery systems are needed to convince governmental and insurance carriers to eliminate the financial barriers to implementing this approach.
Table 4—Methods To Improve PAP Adherence
Category: Apnea
Tags: autoadjusting positive airway pressure, continuous positive airway pressure adherence, obstructive sleep apnea, positive airway pressure treatment