 CPAP delivers a predetermined constant pressure during both inspiration and exhalation (Fig 1). Bilevel PAP delivers a separately adjustable lower expiratory positive airway pressure (EPAP) and higher inspiratory positive airway pressure (IPAP). Bilevel PAP may be more tolerable than CPAP for some patients with difficulty exhaling. The IPAP-EPAP differential is useful for augmenting ventilation in patients with concomitant hypoventilation (“overlap syndrome” and obesity hypoventilation syndrome), and most physicians treat patients with these disorders with bilevel PAP. However, many such patients will also improve with CPAP treatment.
CPAP delivers a predetermined constant pressure during both inspiration and exhalation (Fig 1). Bilevel PAP delivers a separately adjustable lower expiratory positive airway pressure (EPAP) and higher inspiratory positive airway pressure (IPAP). Bilevel PAP may be more tolerable than CPAP for some patients with difficulty exhaling. The IPAP-EPAP differential is useful for augmenting ventilation in patients with concomitant hypoventilation (“overlap syndrome” and obesity hypoventilation syndrome), and most physicians treat patients with these disorders with bilevel PAP. However, many such patients will also improve with CPAP treatment.
Autoadjusting PAP (APAP) devices were developed with two potential uses: (1) autotitrating PAP to select an effective level of CPAP without the need for an attended titration; and (2) autoadjusting PAP for long-term treatment with the advantage of delivering the lowest effective pressure in any circum-stance. Treatment with APAP would also eliminate the requirement for a CPAP titration. APAP algorithms vary between different devices, but in most instances the pressure changes in response to variations in airflow magnitude, airflow limitation, snoring (vibration), and/or airway impedance. The pressure changes gradually between the preset lower and upper pressure limits to avoid inducing arousal (Fig 2). If none of the monitored variables are detected, the device slowly lowers the pressure to a minimum effective setting. Of note, different brands of devices may respond very differently to changes in airflow. Both high airflow leak (mask or mouth), which simulates physiologic events, and the inability to differentiate between central and obstructive apnea by these devices can result in errors in APAP titration. The use of APAP devices for autotitration and the effects of long-term APAP treatment on adherence are discussed below. Recently, autobilevel PAP has been introduced (Fig 3). The physician sets the minimum EPAP, maximum IPAP-EPAP difference (minimum is 3 cm H2O), and the maximum IPAP. The machine then adjusts the EPAP and IPAP to maintain an open airway. The advantages of autobilevel PAP over other PAP modes remains to be demonstrated. However, this mode could potentially be useful in those pressure-intolerant patients who find bilevel PAP alone unacceptable or in patients for whom an effective bilevel pressure is not known.
Expiratory pressure relief (flexible CPAP) is a recent variant of PAP that was developed to improve patient comfort by allowing the airway pressure to fall below the prescribed PAP in early expiration (Fig 1) with a return to the prescribed level at end-exhalation. There are two currently available forms of expiratory pressure relief: C-flex (Respironics; Murrysville, PA) and EPR (ResMed Corporation; Poway, CA). With the C-flex device, the pressure drop is progressively greater on settings 1, 2, and 3, but the amount of drop is determined by a proprietary algorithm based on expiratory flow. With the EPR device, settings of 1, 2, or 3 correspond to pressure drops of 1, 2, or 3 cm H2O, respectively. Flexible PAP is also available with one brand of APAP, bilevel PAP, and autobilevel PAP devices (Respironics). Of note in flexible bilevel PAP the pressure falls at the end of inspiration and the beginning of expiration.
Adaptive servoventilation (ASV) is the most recent variant of PAP. ASV was developed to treat Cheyne-Stokes central apnea in patients with congestive heart failure. However, ASV and bilevel PAP devices with a backup rate are also approved for use with patients with complex sleep apnea (central apnea that persists or appears during a PAP titration). In ASV, a level of EPAP is chosen to keep the upper airway open and the IPAP-EPAP difference adapts between minimum and maximal levels to stabilize ventilation with a goal of providing 90% of the recent average ventilation.  With low tidal volume, the IPAP-EPAP increases; with high tidal volume, the IPAP-EPAP difference decreases. A backup rate triggers an IPAP/EPAP cycle if central apnea is present. ASV is not indicated in patients with hypoventilation and may not be as effective in OSA patients requiring a very high level of EPAP.
With low tidal volume, the IPAP-EPAP increases; with high tidal volume, the IPAP-EPAP difference decreases. A backup rate triggers an IPAP/EPAP cycle if central apnea is present. ASV is not indicated in patients with hypoventilation and may not be as effective in OSA patients requiring a very high level of EPAP.
Today, most PAP devices come with the option of an integrated heated humidification system. Heated humidity can deliver a greater level of moisture than cool humidification and may be especially useful in patients with mouth leak or nasal congestion. Mouth leak can cause a dramatic fall in relative humidity in the mask. This occurs because a one-way flow of air out the mouth allows moisture to escape from the system. This dries the nasal and oral mucosa, which increases nasal resistance. The level of humidity can be adjusted semiquantitatively by the patient. Adequate cleaning of the humidifier chamber and hoses does require extra patient effort. One study suggested that use of humidity is associated with an increase in infectious complications.
For many patients, finding a comfortable interface that does not leak is the major hurdle to adapting to PAP. In our experience, it is not unusual to try several mask types or sizes before finding an appropriate interface. Interfaces include nasal, oronasal (full face), or total face masks; nasal prongs or pillows interfaces that fit in the nares; or an intraoral device’ (Oracle; Fisher & Paykel; Auckland, NZ). Masks have air seals made with either a compliant material that bulges out from pressure or a soft gel material. A small orifice(s) in the mask provides an intentional leak to wash out the exhaled CO2 even at low pressures. Nasal pillows or prongs interfaces may be better tolerated than traditional masks by patients with claustrophobia. Interfaces that fit inside the nostrils (Fig 4) may also provide an effective seal in patients with unusual nasal bridge shapes, those with mustaches, or patients with a lack of support in the area below the nose due to absent dentition. In many patients using a nasal mask, PAP in the nasopharynx moves the soft palate forward against the tongue, thus preventing mouth leak. Other patients must use a chinstrap or oronasal mask to prevent mouth leak. Oronasal masks may be better tolerated by patients with substantial nasal congestion or mouth leak. However, obtaining a good seal with full-face masks is a problem because a large facial area must be sealed. Of note, nasal pillows/prongs interfaces also tend to dilate the external nares and reduce nasal resistance. We have been able to convert some patients with nasal congestion from a full-face mask to a nasal pillows interfaces. A new interface (Hybrid; RespCare; Coconut Creek, FL) is a fusion of nasal pillows and a traditional mask covering the mouth (Fig 4).
PAP treatment is considered the treatment of choice in patients with moderate-to-severe OSA usually defined as an apnea-hypopnea index (AHI) ^15/h. The center for Medicare Services will reimburse CPAP treatment for an AHI > 15/h in patients with or without symptoms. For patients with an AHI > 5 but < 15/h, either symptoms (daytime sleepiness, insomnia, impaired cognition, mood disorders) or comorbid conditions (hypertension, a previous cerebrovascular accident, or ischemic heart disease) must be present for reimbursement.
PAP has been shown to reliably decrease the AHI to levels < 5 to 10/h in patients with moderate-to-severe OSA. Randomized controlled (oral placebo or sham CPAP) studies in this patient group have documented improvement in subjective (Ep-worth sleepiness scale [ESS]) and objective sleepiness. The ESS, an index of propensity to fall asleep in eight situations, has been commonly used to measure improvements in subjective sleepiness on CPAP. Objective sleepiness has been tested using the multiple sleep latency test or the ability to stay awake by the maintenance of wakefulness test.
Clinical experience demonstrates that some symptomatic patients with “milder” OSA (often defined as AHI 4 h per night. In summary, CPAP more reliably reduces the AHI in patients and improves sleepiness as well or better than alternative treatments. Relative patient satisfaction with CPAP vs other treatments likely depends on patient preference.
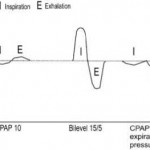
Figure 1. Positive pressure modes: CPAP, bilevel PAP, and CPAP with expiratory pressure relief are illustrated.
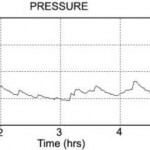
Figure 2. An example of pressure vs time for APAP treatment over a night. The device titrated between upper and lower pressure limits set by the clinician. The average pressure is lower than an optimal fixed pressure. In this case, treatment with a fixed pressure would require a CPAP of 10 to 11 cm H2O.
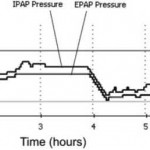
Figure 3. A overnight pressure vs time tracing is shown for a patient using autobilevel PAP with a minimum EPAP of 6 cm H2O and a maximum IPAP of 25 cm H2O. The 90% IPAP and EPAP pressures were 19.2 cm H2O and 16.2 cm H2O, respectively. The average IPAP and EPAP values were 14.6 cm H2O and 11.8 cm H2O, respectively.

Figure 4. Examples of a nasal pillows mask (Swift; ResMed) [left] and a pillows oronasal mask (Hybrid; InnoMed Technologies; Coconut Creek, FL) [right].
Category: Apnea
Tags: autoadjusting positive airway pressure, continuous positive airway pressure adherence, obstructive sleep apnea, positive airway pressure treatment